Anaesthesia for Caesarean Section

Dr. Sandip Sarkar
MBBS, DA, DNB (Anaesthesia & Critical Care)
Consultant Anaesthetist – Institute of Human Reproduction
There are different forms of anaesthesia available for a caesarean section.
You can decide either to go to sleep, known as general anaesthesia, or to stay awake, known as spinal or epidural anaesthesia. The anaesthetic will be given to you by an anaesthetist who is a doctor trained in anaesthesiology. Anaesthetist will discuss the options with you and recommend the best form of anaesthesia for you.
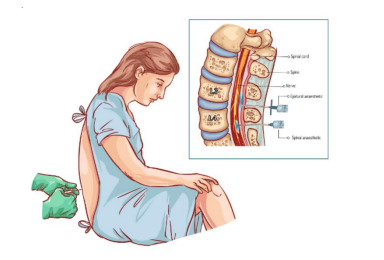
What is spinal anaesthesia?
Spinal anaesthesia, often referred to as a ‘Spinal’, involves injecting anaesthetic and other
painkillers into an area called the subarachnoid space, near your spinal cord. This numbs your nerves
to give pain relief in certain areas of the body.
What happens before spinal anaesthesia?
Before you are given the spinal, the healthcare team will attach some monitors to you that will
measure the Blood pressure, oxygen level, ECG, etc.
Your anaesthetist and the healthcare team will carry out some final checks with you and each other.
Even though you may have been asked some of the questions before, it is important to answer
carefully as the checks are carried out for your own safety.
How is a spinal given?
To insert the needle, your anaesthetist will ask you to either sit up or lie on your side. You will need
to curl up and arch your back as much as possible as this makes it easier for your anaesthetist to
find the right position.
Your anaesthetist will only insert the needle when they are certain that it is in the right position,
then they will inject the anaesthetic through it. They will then remove the needle. You can help your
anaesthetist by keeping still while they insert the needle. It should not be painful you will feel just
a mild discomfort at the back. If you feel pain, let your anaesthetist know.
What effect does a spinal have?
The effect of the spinal can be varied by changing the type and amount of medication given. A
spinal has three main effects.
- Pain relief: The spinal numbs the sensory nerves responsible for pain and touch. This gives pain relief but can also make the area feel numb or heavy.
- Weakness: The nerves supplying muscles will also be affected. This can make it difficult for you to move your legs.
- Low blood pressure: The nerves that help to control blood pressure are also affected. Some women will not be aware of this happening but others may feel sick or light headed if they have low blood pressure. Your anaesthetist will be monitoring you closely for any problems with low blood pressure.
The length of time that the spinal lasts can vary but is usually one to three hours. Your anaesthetist
will put enough anaesthetic through the needle to make sure that it lasts longer than the expected
length of the operation.
What will it feel like during the operation?
You may be aware of pulling and pushing around your abdomen. You may also feel short of breath
because the sensory nerves around your chest will be numb. This does not mean that there is any
problem with your breathing.
What are the benefits of a spinal?
Compared to a general anaesthetic, a spinal has benefits to both you and your baby. As you are awake, you and your partner can share in the birth and your baby can be brought to you shortly after delivery.
You can breastfeed soon after the delivery.
A spinal is safer than a general anaesthetic, although both types are safe.
Recovery is usually more comfortable and quicker.
There are no significant side effects for you or your baby.
What complications can happen?
Your anaesthetist will try to make the spinal as safe as possible but still, complications can happen.
The possible complications of a spinal are listed below.
- Failure of the spinal: Most spinals work well first time but sometimes they do not. Your anaesthetist may repeat the injection or discuss with you other options such as a general anaesthetic.
- Itching: This can occur if morphine or similar drugs are given in spinal. The effect is usually mild and easily treatable.
- Low blood pressure: The risk depends on your medical condition and the type of medication used. It is usually treated and you will be closely monitored by your anaesthetist. Sometimes the first sign of a fall in blood pressure is feeling sick or light-headed. It is important that you let your anaesthetist know straight away if this happens.
- Difficulty passing urine: This is because the nerves to your bladder are numbed. You will have a catheter, which is a small tube, inserted into your bladder to help you pass urine.
- Headache: This is common after an operation the risk of which is 1 in 100. This headache can vary from mild to severe and can be treated. To minimise the risk of post spinal headache special pencil point type needles are used now a days.
- Backache: This is common after an operation incidence is around 10%. It is common to have a bruised feeling for a few days where the spinal was inserted. There is no evidence that having a straightforward spinal causes long-term backache.
- Blood clots, also known as Haematoma: The risk of developing a blood clot is 1 in 200,000.
- Nerve damage: The risk for developing nerve damage is 1 in 23,000. This is not usually serious and gets better.
- Unexpected high block: If the local anaesthetic spreads beyond the intended area (the risk for which is 1 in 2,000), it can cause difficulty in breathing, low blood pressure and rarely causes unconsciousness.
General Anaesthesia
What is general anaesthesia?
A general anaesthetic is a combination of drugs that causes deep sleep. It is used for operations or
procedures as it causes a reversible loss of consciousness. You will not be aware of what is
happening and afterward, you will not remember anything that happened.
What happens before general anaesthesia?

Before you are given the anaesthetic, the healthcare team will attach some monitors to you that
measure your blood pressure and the amount of oxygen in your blood. If you need oxygen, they
will give it to you through a mask or small tube in your nostrils.
Your anaesthetist and the healthcare team will carry out some final checks with you and each other.
Even though you may have been asked some of the questions before, it is important to answer
carefully as the checks are carried out for your own safety.
How is general anaesthesia given?
Most people are sent to sleep by injecting the anaesthetic through a cannula, which is a small tube
inserted in a vein. It takes around 30 seconds to work. The injection can ache a bit at the time but
any discomfort will be gone when you wake up.
Before you go to sleep, your anaesthetist will ask you to breathe oxygen through a face mask. As
you go to sleep you will feel the assistant pressing firmly on the front of your neck. This is to prevent
anything in your stomach from passing up into your lungs. To help protect your lungs during the
operation, your anaesthetist will place a breathing tube called an endotracheal tube into your windpipe,
known as the Trachea. This will be removed at the end of the operation when you are awake.
You will be kept asleep by breathing anaesthetic gases. Your anaesthetist will monitor you closely.
When the operation has finished, the anaesthetic wears off, allowing you to wake up again.
What complications can happen?
Your anaesthetist will try to make the general anaesthetic as safe as possible but complications can
happen. Some of these can be serious. The possible complications of a general anaesthetic are listed
below.
Your anaesthetist may be able to tell you if the risk of a complication is higher or lower for you.
- Nausea or vomiting after the operation: The risk of nausea or vomiting is around 30%. The risk is higher with certain people and certain operations but can be reduced with medication given either by your anaesthetist at the time of giving general anaesthesia, or by the ward doctor after the operation. If you think you may be prone to being sick, let your anaesthetist know.
- Sore throat: The risk of developing a sore throat is 1 in 6 and this usually gets better quickly.
- Headache: The risk of developing a headache is 1 in 20 and is not usually severe and settles with time. Simple painkillers such as paracetamol may help.
- Muscle and back pains: This can be caused by the medication used or being in one position during the operation. The risk of developing muscle or back pain is 1 in 20. If you know that certain positions are likely to cause problems, let you anaesthetist know.
- Dental damage: The risk of damage to the front teeth or any crowns is less than 1 in 100. Your anaesthetist will always ask to look inside your mouth. Let them know if you have any loose teeth, crowns or bridgework.
- Difficulty passing urine: You may need a catheter in your bladder for one or two days.
- Breathing difficulties: Your anaesthetist may have difficulty placing the breathing tube in your windpipe. The risk of this happening is 1 in 100. They may need to wake you before you have the caesarean section and recommend an alternative technique for you. The risk of this being necessary is 1 in 1,000.
- Awareness during the operation: The risk of this occurring is 1 in 200.
What effects are there on the baby?
Some anaesthetic will pass from you to your baby. This may make your baby drowsy for a short
while but there are no long-term effects. You will not be able to hold your baby or breastfeed until
you are awake enough.
Summary
Both spinal and general anaesthesia for caesarean section is usually safe and effective but
complications can occur in both. General anaesthesia has the advantage of rapid induction, reliability,
less chance of fall in blood pressure. Spinal anaesthesia has the advantage of being a simple technique,
minimal risk to the baby, a minimum hazard of aspiration. In Conclusion, Spinal anaesthesia is
considered simple and safer than other techniques of anaesthesia for caesarean delivery and is, therefore, the technique of choice of most Anaesthesiologists.